In vivo Differentiation of Myocardial Ablation lesions via a Stiffness ratio with Acoustic Radiation Force Impulse Imaging
Stephanie A. Eyerly1, Stephen J. Hsu1, and Gregg E. Trahey1, and Patrick D. Wolf1
1 Duke University, 136 Hudson Hall, Durham, NC, USA
Background
Acoustic radiation force impulse (ARFI) imaging has been shown to be capable of visualizing cardiac radiofrequency ablation (RFA) lesions in myocardium based on ARFI-induced displacements[1]. Current lesion segmentation methods successfully threshold normalized ARFI-induced displacements based on user defined parameters to visualize the boundary of the lesion, but these methods may be biased by subjective variability. Stiffer, ablated tissue has been shown to undergo only moderate elasticity changes throughout the cardiac cycle unlike the surrounding, untreated myocardium[2]. This fact suggests that the intrinsic cyclic stiffening of the myocardium could facilitate the formulation of a systolic to diastolic normalization for ARFI-induced displacement data.
Aims
To automatically normalize and detect ablation lesions in ARFI-induced displacement images based on changes, or lack thereof, in myocardial elasticity from systole to diastole.
Methods
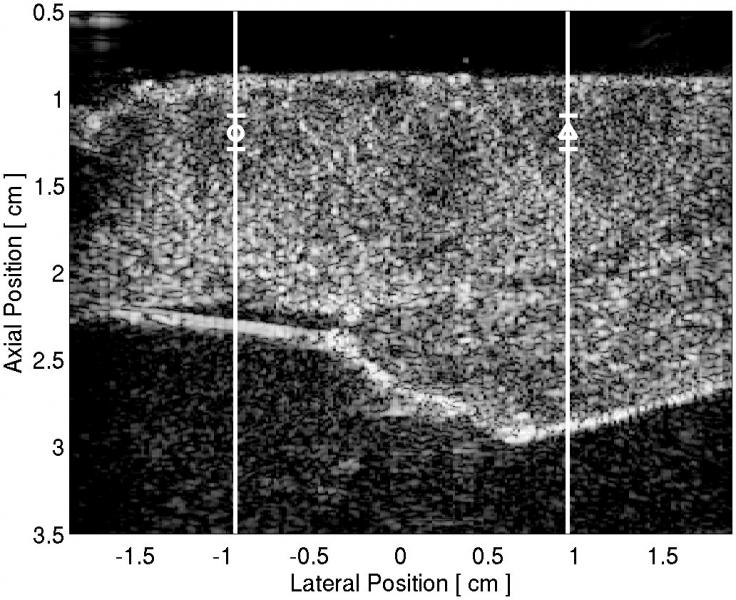
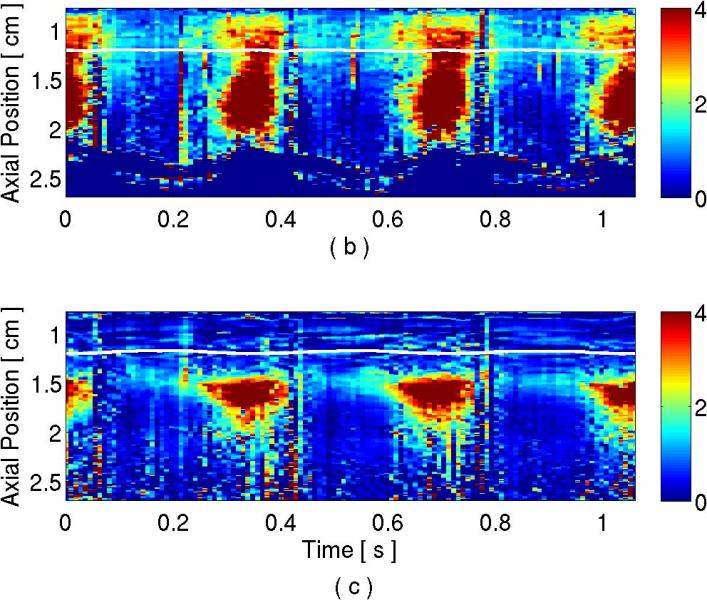
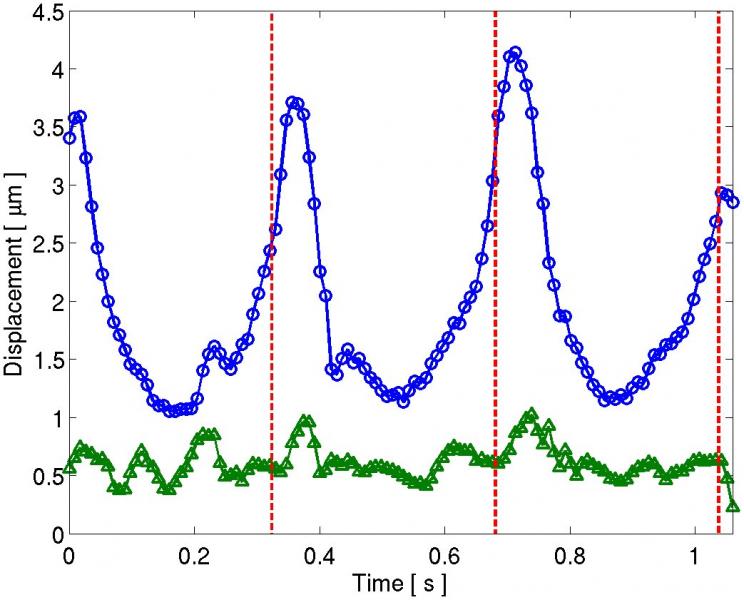
A canine heart was imaged epicardially in vivo using with an open chest preparation. An ablation lesion was created on the epicardial surface, and a transducer, held in place using a vacuum-coupling device, was positioned directly above the lesion and along the long axis of the heart. While pacing from the ventricular surface, two-line M-mode ARFI images were acquired at 120 Hz for multiple cardiac cycles. 1-D speckle tracking was employed to follow specific regions of myocardium through time for each M-mode line, one inside and one outside the ablation lesion. An average diastolic to systolic ARFI-induced displacement ratio for the each line was formulated.
Results
Image
| Image
| Image
|
| Figure 1: (a) B-mode image of the LV free-wall. Vertical white lines indicate the locations of the M-mode lines situated outside (circle) and inside the lesion (triangle). M-mode ARFI images showing displacement in microns over time and depth for the (b) line through untreated tissue and (c) the line through the lesion. The stiffness of the lesion is visible by low displacements maintained at the tissue surface throughout the cardiac cycle. The horizontal white lines mark 1-D speckle-tracked lines through time in a region of myocardium at the depth of the lesion. The ARFI-induced displacements along this speckle-tracked line are plotted in (d), where the circle and triangle plots correspond to the M-mode lines outside and inside the lesion, respectively. The red dashed lines indicate the external pacing stimulus time. For each curve, a systolic to diastolic stiffness ratio was calculated. | ||
Conclusions
The analysis of the M-mode ARFI image of the ablation lesion throughout the cardiac cycle indicated that the stiffer ablated tissue displayed only a slight change in elasticity between systole and diastole with a ratio 1.5:1, while the surrounding untreated myocardium experienced a greater change in elasticity with a ratio of 2.9:1. Once ECG-gated ARFI images are acquired at systole and diastole, these stiffness ratios can be calculated for the entire field and potentially used to automatically demarcate the extent of an ablation lesion.
Acknowledgements
This research was funded by NIH Grant #: R21-EB-007741. We would like to thank Siemens Medical Solutions USA, Inc. for their hardware and system support.
References
[1] B Fahey, K Nightingale, P Wolf, and G Trahey. Acoustic radiation force impulse imaging of myocardial radiofrequency ablation: Initial in vivo results. IEEE Transactions on Ultrasonics, Ferroelectronics and Frequency Control, 52(4):631-641, 2005.
[2] S Hsu, R Bouchard, D Dumont, P Wolf, and G Trahey. In vivo assessment of myocardial stiffness with acoustic radiation force impulse imaging. Ultrasound Med Biol, 33(11):1706-1719, Nov 2007.