On the Assessment of Radiofrequency Ablation lesion size with Acoustic Radiation Force Impulse Imaging
SA Eyerly1*, SJ Hsu1, GE Trahey1, SH Agashe1, Y Li1, PD Wolf1
1 Duke University, Durham, NC, USA
Background
Ablation has become the preferred treatment for most cardiac tachyarrhythmias. Several studies have investigated the use of acoustic radiation force impulse (ARFI) imaging to visualize lesions created from these ablation procedures.1,2 ARFI imaging has been demonstrated to be a suitable imaging modality in determining lesion size and continuity, as there is a high contrast in stiffness between the ablation lesion and the surrounding untreated tissue. However, an exact quantitative assessment into the accuracy of ARFI imaging of ablation lesions has not been performed.
Aims
To quantify, in vitro, the ability of ARFI imaging to determine the size and extent of ablation lesions within myocardial tissue.
Methods
An ablation chamber was built such that lesions, created by radiofrequency ablation (RFA) in excised myocardium, could be imaged with an intracardiac catheter and precise control of the imaging plane. Alignment slits were present so that the imaging probe could be properly aligned within a specific imaging plane. These slits were then used as guides when sectioning the identical slice plane for pathology. The lesion was then photographed along the cut plane and manually segmented based off visible discoloration within the myocardium. Once registered with the acquired B-mode and ARFI images, the sensitivity and specificity of the corresponding ARFI images were determined.
Results
Image
a) | Image
 c) |
Image
 c) | Image
 d) |
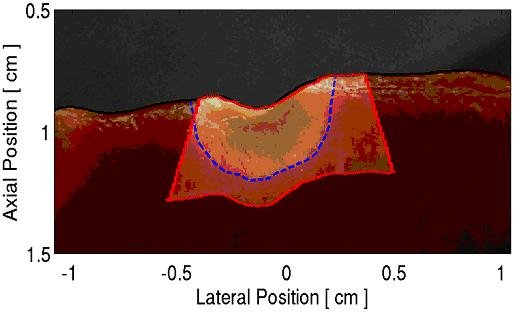
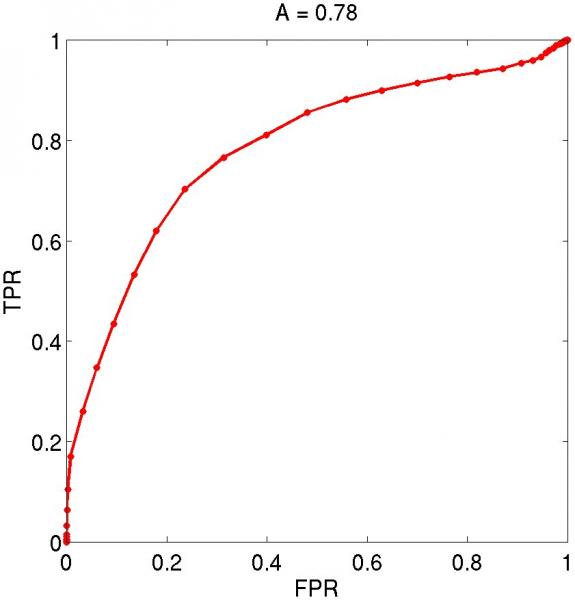
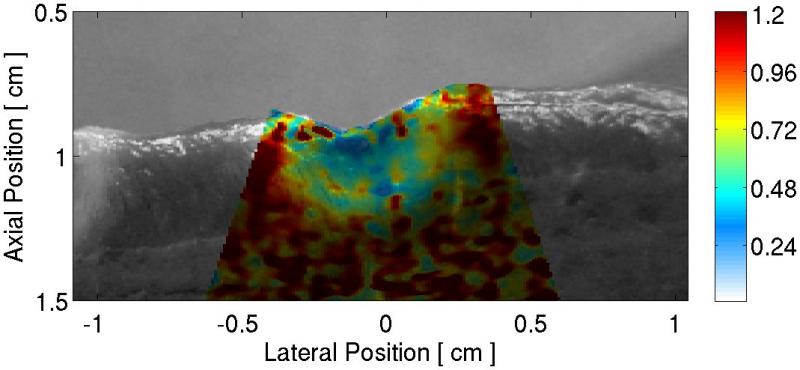
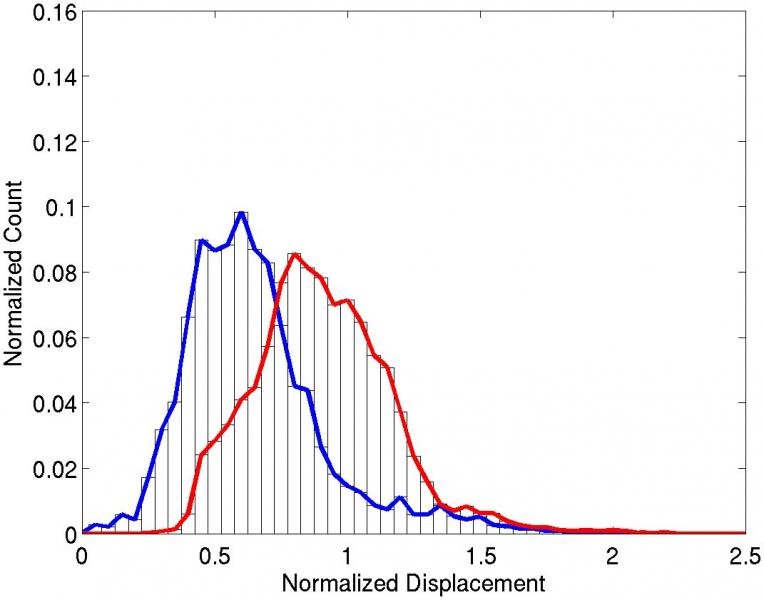
Figure 1: A typical result from these experiments is presented. (a) The pathology slice of a RFA ablation lesion is shown with (b) the co-registered ARFI image. Using time-gain compensation based methods1, displacements within the ARFI image have been normalized with depth. By segmenting lesion boundaries based on visible tissue discoloration, probability density functions (c) show average normalized displacements within the lesion (blue plot) and surrounding tissue (red plot) to be: 0.58 - 0.35, and 0.91 - 0.26, respectively. Receiver operating characteristics analysis (d) indicates an accuracy of 78% in segmentation of the lesion with ARFI imaging.
Conclusions
We have developed a hardware and software system that provided image plane co-registration between an ultrasound system and a pathology photograph. Using this system, ARFI ultrasound images of ablation lesions were directly compared with photographs of the pathology. Analysis of additional lesions for training will allow us to identify thresholds for ARFI parameters for optimal differentiation of tissue in a real time system.
Acknowledgements
This research was funded by NIH Grants #: R01-HL-075485, R01-CA-114093, and R21-EB-007741. We would like to thank Siemens Medical Solutions USA, Inc. for their hardware and system support.
References
[1] Fahey BJ, Nightingale KR, Wolf PD, and Trahey GE. Acoustic radiation force impulse imaging of myocardial radiofrequency ablation: Initial in vivo results. IEEE Trans on Ultrason, Ferroelec, and Freq Contr. 52, 631-41, (2005).
[2] Hsu SJ, Fahey BJ, Dumont DM, Wolf PD, and Trahey GE. Challenges and implementation of radiation force imaging with an intra-cardiac ultrasound transducer. IEEE Trans on Ultrason, Ferroelect, and Freq Cont 54, 996-1009, (2007).